It’s 9am on a cold, clear winter morning in Calton, Glasgow, and Harry* has been waiting for The Thistle to open. He’s not in great shape – in a wheelchair with one leg missing, he’s been sleeping rough and looks like he’s been doing so for a while. In the sub-zero weather, he only has one safe, warm place to go, so when the sliding doors to the UK’s first safer drug consumption facility open, he’s the first one in.
His face cracks into a smile when he sees a team of familiar faces behind the reception desk standing below a sign that says “Welcome”.
“Hiya, Harry,” one young man in scrubs says. A red-headed nurse asks: “You freezing, Harry?”
“Yeah,” he says. “Feel my hand.”
“Aye, you’re freezing. Let’s get you inside.”
She buzzes open a door marked “Using space”, where Harry will find a reception desk and eight mirrored booths where, if he so wishes, he can inject himself with his own drugs. It’s a clinical room, with grey floors and white cupboards. On the desk there’s a sterilised needle, which Harry can use at an allocated booth (No 1 is the favourite because it’s furthest away from the staff).
If he appears to be looking for a vein in a high-risk area – say neck or groin – he’ll be given an infrared vein finder so he can find one in his arm. If the worst happens and he overdoses, the staff will grab one of the crash mats hidden behind the cupboards and inject him with naloxone to resuscitate him and save his life.
Since it opened on January 13, 2025, The Thistle has been accessed 10,819 times – 7,460 times to inject drugs. Out of those episodes, there’s been 88 overdoses/medical emergencies but no fatalities, and an ambulance has been called 15 times.



But today, Harry isn’t doing any of that. He’s heading straight to the “lounge”, where there are comfortable sofas, a TV, free tea and coffee and plenty of books, games and puzzles. There are flyers and posters encouraging people to access support and rehabilitation, and a whiteboard lists the week’s services, including GP visits, dental van availability and sexual health clinic opening hours. Opposite, on a coffee table, people write their hopes, dreams and ambitions on a tree of life.
“Wish my kids are doing well and enjoying secondary,” one tag reads. “Thank you for all the love and support every staff member has shown me,” reads another. “It has made me realise my potential again.”
“Stable lifestyle. Settled home. Relationship and enjoy life xx.”
“Hope to be clean by this time next year.”
“Sort my shit out! And get house ASAP.”
“To love and be loved.”
Scotland has the highest rate of drug-related deaths in Europe – by a long way, and for a long time. Rapid Action Drug Alerts and Response’s quarterly report found drug deaths in Scotland averaged 24 per week between March and May 2025. In the past decade, 10,884 people have died from drug misuse, a figure which leaves an indelible scar on a small population of 5.5 million.
Families and communities are ripped apart; parents lose their children and children lose their parents. Many turn to substances to cope with the trauma, and the cycle continues.
Service manager Lynn Macdonald says The Thistle aims to break that cycle. “For some people, their visit can prompt the conversation about going into treatment, perhaps looking at detox options and seeing what else is out there,” she tells me.
One of the many criticisms levelled at The Thistle over the past year is that none of the service users have gone into rehabilitation. But Macdonald says their focus is on harm reduction, and The Thistle is just the very first step on a long road to rehabilitation and recovery.
“Trust is a huge part of what we do,” she says. “People haven’t had good experiences of public health services, so we’re trying to change that. We welcome people in and treat them as equals, as you and I would expect to be treated if we walked into any kind of healthcare setting. We’re giving people their dignity back.”
For people like Harry, this may be the first time they’ve had a positive experience with healthcare staff – a crucial step towards rebuilding trust and planting a seed of hope that may well bear fruit.
Suggested Reading


How to shout at the NHS
The Morrisons supermarket around the corner is often at the centre of this debate. Its sprawling car park is a popular spot for drug users, and local press and the public regularly report piles of discarded needles and foil scattered all over the concrete and edges.
The local press claim it has got much worse since The Thistle opened. However, councillor Allan Casey, City Convener for Addiction Services, says it has always been a problem area, and that’s why The Thistle was placed nearby in the first place.
“The number of times people have accessed the service is around 10,000,” he tells me. “That’s 10,000 times where people aren’t injecting in the streets, public alleyways, parks or open spaces. So I really do think that that has made a significant difference in the local community.”
Recently, representatives of the Morrisons branch in question gave evidence in the Scottish Parliament. “The official reported a 94% decrease in the number of discarded needles on their land,” says Casey. “Now, that’s huge.”
So I headed over to Morrisons to ask the in-store manager what that looks like in practice. “Every two or three months we get a specialist out to clean the needles and all sorts from the edge of the car park,” he says. “It stresses the customers out, aye.”
And as The Thistle is only open from 9am-9pm, the local community still struggles with the impact. One man who owns a garage nearby describes The Thistle’s opening as “hell.”
“My office is right there,” he says, pointing to a small room with a laptop. “Last month, I found someone in there trying to nick my computer.”
He lives nearby and says his children found a needle covered in blood in their backyard, and when I ask him if it’s got worse since The Thistle opened he gives a resounding yes. “If it were up to me,” he says, “I’d line all the addicts up and shoot ’em.”
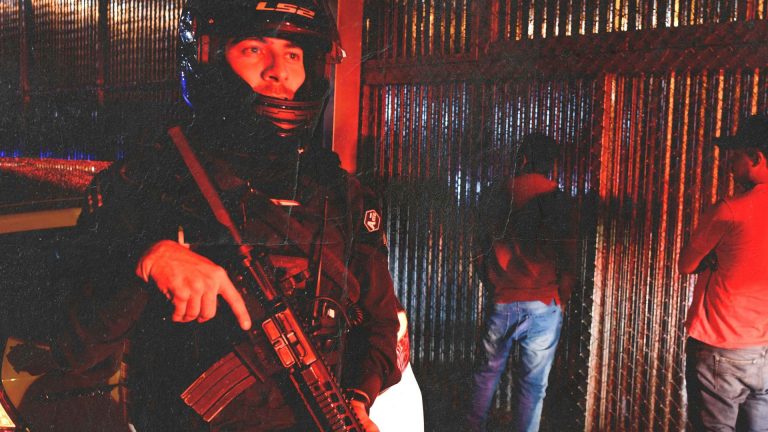
Scotland’s drug problem became prominent in the 1980s. As key industries like shipbuilding and manufacturing declined, many were left destitute and jobless. Simultaneously, the Scottish government de-prioritised crucial public health services and institutions, leaving many poverty-stricken communities without support. Then volatility in countries like Afghanistan and Iran led to excessive supplies of heroin flowing into Europe at bargain rates.
Scotland wasn’t equipped for the crisis, and the response was slow and hostile. Drug users were criminalised and demonised, with the country pointing blame at the individual rather than viewing it as a public health crisis. But Kirsten Horsburgh, CEO of Scottish Drugs Forum, says that’s exactly what it is, and must be addressed as such.
“That means we must respond with compassion,” she says. “Every single person who works in The Thistle works there because they believe in people. They want people to do well. And when people have a lack of hope and self worth, even just the really small acts of kindness can have a massive impact on their lives.”
According to the Scottish Health Survey, prevalence rates of trauma exposure among individuals with substance-use disorders are as high as 97.4% in some areas of Scotland. Adults who experienced four or more adverse childhood experiences are 16 times more likely to use crack or heroin.
“Really, [The Thistle] is just a compassionate approach to substance use,” Horsburgh says. “So if people are injecting in outdoor, unsafe locations, safer consumption facilities offer a space where they can be treated with dignity and respect and able to use their drugs in a safe environment, and also have access to healthcare.”
Suggested Reading
The end of the Costa Rican dream
Taking a compassion-led, harm-reduction approach to addiction might be progressive by British standards, but it’s nothing new. The first safer drug consumption facility was established in Bern, Switzerland, in 1986.
Since then, over 200 facilities have opened across Europe, including in the Netherlands, Germany, Denmark, Spain, and Portugal. In Catalonia, you’ll find them in the form of “social cafes” – safe, welcoming third spaces with affordable or free food and coffee where support workers mill about offering informal contact and referrals.
The idea is simple: to fight addiction through community and connection.
With funding secured for two more years, The Thistle hopes to expand to include an inhalation room and a drug testing service. But in order for the impact to reach the wider community, Horsburgh says the UK needs more facilities.
“We’re really behind the times in the UK,” she says. “It’s so disappointing that the government won’t enable these facilities to happen more easily. It’s not about injecting, it’s about connecting. And that’s really what this is for.”
*Name changed to protect anonymity
Alice Austin is a freelance journalist whose work has appeared in the Guardian and on the BBC.